Osteochondrosis of the cervical spine is a disease that develops in adults after the age of 25 due to structural changes in cartilage tissue. In the fairer sex, the disease develops more often due to the peculiarities of the hormonal background. We all need to know the symptoms of cervical osteochondrosis in women in order to diagnose the disease in a timely manner and immediately begin complex treatment.
An exact diagnosis can only be made by a doctor. An experienced neurologist is involved in the treatment. He commissions additional studies to determine not only the stage of development of the disease, but also the cause of its development. Then it will be much easier to choose the optimal regimen of therapy to save the patient from the main manifestations of the disease.
Obvious signs of osteochondrosis of the cervical spine in women appear when the disease is already actively developing in the body. The slightest disturbance of well-being is a reason to see a doctor. If you run into the problem, osteochondrosis will turn into protrusion or hernia over time. The patient is on the operating table. The consequences of the disease persist for life. At an early stage in the development of the disease, its symptoms can be completely eliminated. It is in your power to improve your health and ensure an active, full future for yourself without injury, dystrophic tissue changes, and constant pain.
What is osteochondrosis?
Osteochondrosis is a common disease that is characterized by changes in the structure of the cartilage tissue in the intervertebral discs. This disease can affect any joint, but most commonly the spine. There are clear signs of osteochondrosis in women, but definitive conclusions about the development of the disease can only be drawn after a comprehensive diagnosis.
The cervical spine is considered to be the most flexible. This area is often prone to various dystrophic lesions because it is the least protected. There are no large muscles protecting and supporting the spine. The division consists of seven separate vertebrae. They are based on bone tissue. Between each vertebra there is a soft "layer" - the intervertebral disc, which provides flexibility and mobility to the neck. Hormones play a big role in the structure of the tissue, therefore osteochondrosis develops differently in women and men.
According to statistics, 60-70% of the mature population of the planet suffer from this disease, and in 30% of cases, the cause of constant headaches, migraine is precisely osteochondrosis of the cervical spine.
To understand when to see a doctor, you need to study the list of symptoms of the disease.
Why osteochondrosis is dangerous for women

The main symptoms of osteochondrosis in women are considered in more detail, since the weaker sex suffers more from the disease.
This is due to the structure of the female body:
- Muscle tissue is not as developed and pumped out in women as it is in men. This is an aggravating factor in the development of the disease.
- Women are more likely to work in the office and spend a lot of time in one position at the computer.
- The hormonal background of the female body is radically different from that of the man. During menopause, dystrophic changes in the thickness of the cartilage tissue become more pronounced.
In adulthood, women gradually deteriorate bone tissue. This is due to the development of osteoporosis. Calcium is washed out of the bones and its reserves are not replenished. The female body no longer produces a special hormone that promotes the absorption of the trace element. If both cartilage and bone are destroyed at the same time, the consequences can be serious.
For this reason, women over 40-45 years of age are recommended to have blood calcium tests annually to check the condition of bones and cartilage. Certain preventive measures will help eliminate the manifestations of the disease and restore the integrity of the cervical spine in a timely manner.
With osteochondrosis, the structure of the cartilage tissue changes, it becomes denser and more rigid. The flexibility and mobility of the vertebrae is lost. When this disease passes into the intervertebral weight, the contents of the disc protrude beyond the annulus fibrosus. Getting rid of such a complication without surgery is problematic. It is not worth bringing into such a state. Try to monitor your health.
The main manifestations of the disease at an early stage
The signs of cervical osteochondrosis in women differ in the early stages and in the late stages of development. At first, the disease is almost not annoying, but it is still worth paying attention to minor symptoms.
This list contains:

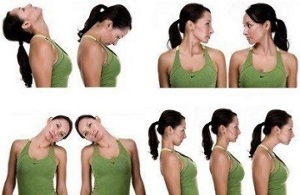
- neck discomfort, especially in the morning;
- crunching with circular movements of the head, bent to the side;
- Frequent headaches;
- Slight dizziness with a sharp turn of the head to the side.
Due to structural changes in the tissue, the roots of the nerve endings are pinched, which leads to headaches.
The neck is no longer flexible. Women are often observed to move forward.
It is more and more difficult to maintain the posture, sometimes there is even a slight hump at the transition from the neck to the shoulder girdle. All of this clearly shows the development of osteochondrosis.
Instead of making an appointment with a neurologist, women complete numerous massage courses. This effect has a short-term effect. If you do the massage incorrectly, it will damage the body even more over time.
Specificity of the course of cervical osteochondrosis
Osteochondrosis of the cervical spine in women can be asymptomatic for a long time. The limited mobility of the neck is attributed to fatigue, muscle constipation and headaches, which are not yet very bothersome. And when they do occur they call them the culprit, stress, poor sleep. A provoking factor in the transition of the disease from a latent to an acute form can be sharp hypothermia and a slight injury. Often times, the disease develops at a reactive rate. Yesterday the woman still felt fine, but today she cannot take her head off the pillow because of severe pain. Don't expect this condition to go away on its own. Hurry up to see a doctor. Even at this stage, you can completely eliminate the manifestations of osteochondrosis and provoke its factors.
It is strictly forbidden to contact bone setters and osteopaths. In official medicine there is no such thing as "reduction of the vertebrae". Such aspiring specialists will only hurt. Due to excessive mechanical stress, cracks can appear in the thickness of the cartilage and bone tissue. During the first session with an osteopath, you will really feel better, but all of his actions over time will only result in osteochondrosis becoming a major hernia.
The traditional treatment consists of several phases and is always carried out consistently and without pain. Any activity is prohibited during the acute period. To avoid restricted mobility and severe pain, all you need to do is listen to the main recommendations of your doctor. can be observed by a neurologist and a vertebrate at the same time. These highly qualified doctors with advanced medical training implement complex treatment methods.
Acute symptoms
When the disease becomes acute, the symptoms of cervical chondrosis in women change.
At this stage, the overgrown cartilage tissues press on the nerve endings, pressing the large arteries along the spine to the brain and feeding it. Lack of oxygen manifests itself in frequent fainting. Possible loss of short-term memory, disorientation in space.
By pinching nerve endings, limb sensitivity is lost. A feeling of numbness in the shoulder girdle, tingling in the fingers is very alarming.
If you do not start treatment quickly at this point, there is a possibility of partial paralysis. The patient stops feeling the upper limbs as a whole.
If you consult a doctor at this point, all of his efforts will initially be directed towards stabilizing the patient's condition.
After weaning from the acute period of illness, various therapy methods are prescribed, including taking medication and various physiotherapy procedures.
Movement therapy is very effective when classes are given by a certified instructor who has sufficient experience in rehabilitation of patients with spinal injuries.
Diagnostic methods
The diagnosis of osteochondrosis of the cervical spine is comprehensive. The first time you see a doctor, describe in detail any bothersome symptoms. Already on the basis of this information, the doctor can draw certain conclusions about the development of the disease. The final diagnosis can only be made after additional examinations. Innovative functional diagnosis methods are increasingly being used in medical practice. These include computed tomography and magnetic resonance imaging. With the help of a special device, the tissues of the spine are examined in real time. With this technique you can create three-dimensional images in different projections, thoroughly examine an organ, system or department. The patient receives images and slices with the examination protocol. The diagnostician makes a detailed description, but your doctor is responsible for the final decoding.
Using these examinations, it is already possible to assess the degree of development of the disease, the affected segments of the intervertebral discs. Check-ups are carried out every six months to assess the dynamics of treatment.
Sometimes additional biochemical blood tests are prescribed. They help to understand whether an inflammatory process is developing in the body.
MRI or X-ray

Some patients complain that MRI or CT are too expensive. In most cases, such an examination is carried out for a fee, since high-quality, high-performance equipment is expensive and used in private diagnostic centers. With patients, of course, the question arises whether regular x-rays are possible.
Only a panoramic x-ray can provide certain information about the development of the disease.
The cost of this procedure is not much lower than an MRI or CT scan. Bone tissue is clearly visible here, but it is problematic to draw reasonable conclusions about the condition of the cartilage and connective tissue. That is why specialists prescribe more modern diagnostic methods. You shouldn't refuse them as magnetic resonance imaging is also much safer. It can be done several times at short intervals as no hazardous radiation is used in the study.
is it possible to get rid of osteochondrosis forever?
Knowing the main symptoms and manifestations of cervical osteochondrosis in women will make it much easier for you to get rid of the disease. The earlier the patient turns to the doctor, the greater the chances of successful and rapid healing.
A complex of anti-inflammatory, decongestant drugs, the active use of drugs based on natural collagen that increase the elasticity of connective tissue, nutritional corrections, moderate physical activity and exercise therapy are the main areas of treatment.
Only by correcting the usual way of life and changing attitudes towards physical activity can you achieve positive results.
Prevention
Since it is known that osteochondrosis of the cervical spine is common in women, it is advisable to take preventive measures to prevent this complex disease from intensifying. If you play sports, eat right, run a lot in the fresh air, monitor all systems and functions in the body, the disease will never overtake you.
If you work out in the gym, do so under the supervision of an experienced qualified trainer who will always make sure that the basic exercises are followed.
Yoga and Pilates courses help prevent osteochondrosis.
Signs of osteochondrosis are already visible in the early stages of the development of the disease. It is important not to miss them and to start treatment on time so that the health of the musculoskeletal system is guaranteed.



























